History of the EHR: A Practice in Problems and Paper


History of the EHR: A Practice in Problems and Paper
Let’s take a walk through (medical) history — and how it shaped our love-hate relationship with the EHR.




Table of Contents
Is the EHR just a paper record in a digital trench coat?
Kind of. Electronic health records (EHRs) were supposed to solve paper charting’s problems:
“By computerizing health records, we can avoid dangerous medical mistakes, reduce costs, and improve care.”
— President George W. Bush, 2004 State of the Union Address
It’s a hard promise to keep. Instead of fixing the system, EHRs digitized the cracks.
But the story’s not over yet. Let’s take a walk through (medical) history — and how it shaped our love-hate relationship with the EHR.
Who knows? Maybe there’s a happy ending.
Paper in practice
Paper notes had a problem — and it wasn’t just bad handwriting.
In 1971, Dr. Larry Weed spoke to Emory University. He flipped through a “typical medical chart, thick as a phone book” and told a room full of physicians why their notes didn’t work.
"The human mind simply cannot carry all of the information about all of the patients in the practice.” — Dr. Larry Weed
Charts were a hodgepodge of scribbles and abbreviations. They jogged your memory, while everything else lived in your head.
As a scientist first, Weed knew how to collect data. He noticed a pattern of:
- Miscommunication
- Missing context
- Solutions without a clear problem
He came up with the Problem-oriented Medical Record (PoMR), and clinicians got a new favorite acronym (right behind RRR).
But really, we were piecing together medical history.
“This is the practice of medicine. It determines what you do in the long run. You’re a victim of it, or you’re a triumph because of it.” — Dr. Larry Weed
Making progress
Ten years later, progress notes were part of the job — along with Weed’s SOAP format (or method to the madness).
Of course, it wasn’t perfect. Charts were hard to read or covered in coffee stains. Here’s how one Reddit user described charting before the EHR:
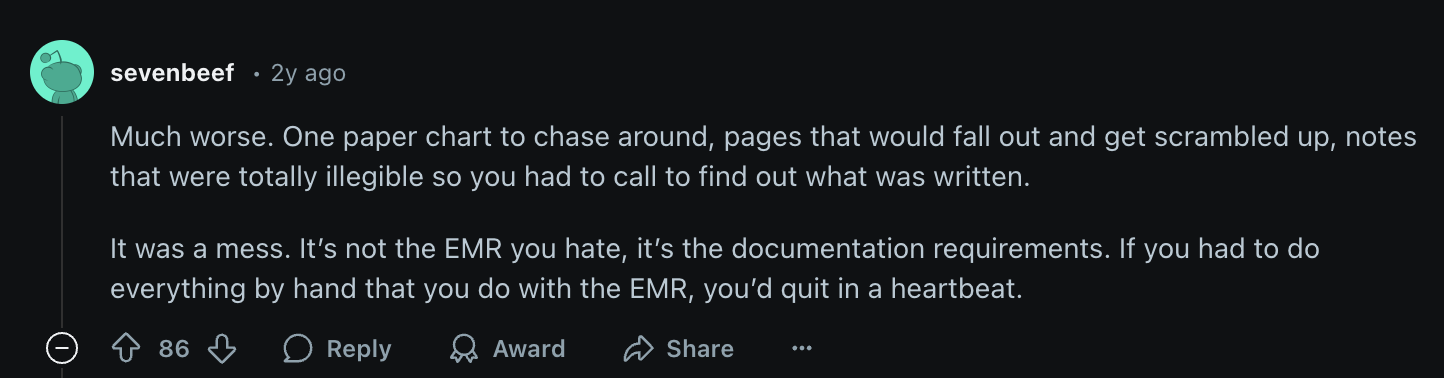
This gets us to the real problem: Charting is a full-time job, and it’s not the one you signed up for.
The shift from paper didn’t lighten the load. It just changed the format.
The digital shift
Electronic records first showed up in hospitals and large academic centers. By the 90s, they were in most clinics.
This was a bit of a “will they/won’t they” situation. EHRs were meant to “complement, not replace the paper chart.” So, we juggled two records instead of one.
That changed in 2000: President Bush doubled funding, set interoperability standards, and asked the country to get on board.
Ten years later, they stopped asking. The “Health Information Technology for Economic and Clinical Health” (HITECH) Act mandated the EHR for the first time.
Of course, that’s not the end of the story.
EHRs today: A love-hate relationship
Today, EHRs are everywhere — but so are their problems.
The Love:
- Instant access to patient records: No more searching through paper files
- Medication safety alerts: Preventing dangerous drug interactions
- Built-in decision support: Flagging abnormal lab values and missed screenings
The Hate:
- Too many clicks: Are we navigating an EHR or hacking the Pentagon?
- No interoperability: Your patient’s data is trapped in someone else’s system with few EHR integrations.
- More documentation, not less: Turning physicians into high-paid data entry clerks.
As one physician put it:
"I visited a new doctor, and he needed my past lab results. Both doctors used Epic. Could he pull them up? No. For some obscure reason, I had to track them down myself." — Kevin Davidson, 36 years in EMR development
EHRs were supposed to cut administrative work. Instead, they created a new kind of burden.
A PhD in admin work
Where there’s an EHR, there’s pajama time.
"Instead of fixing medicine, EHRs turned doctors into the highest-paid data entry clerks in the country."— Dr. Abraham Verghese, The New York Times
You don’t log in after hours because you want to. You do it because documentation isn’t built for the pace of patient care.
The chart lags behind the conversation, the clicks pile up, and before you know it, work follows you home.
The fix isn’t more time — it’s less work.
“If I don’t click fast enough, meds get delayed. If another patient needs me later, I’m already exhausted. All because my EHR demands midnight paperwork” — Dr. Briga Mullin, Hospitalist
Making medical history
The history of the EHR is still being written. The goal? To create a system that works for clinicians, not against them.
The problem isn’t the EHR: it’s too much documentation. Fixing it means offloading the work clinicians were never meant to do.
AI and the new frontier
Unlike traditional EHRs, AI tools don’t just store information — they process it. They’re designed to capture conversations, write notes, and support interoperability, so clinicians don’t have to click through their entire shift.
- AI scribes listen in real-time and generate structured notes.
- Automated summaries surface key patient history without endless scrolling.
- Interoperability solutions use AI to bridge the gaps between disconnected systems.
For decades, clinicians have had to learn new systems. It’s time for tools to adapt to the practice of medicine, not the other way around.
FAQs
Frequently asked questions from clinicians and medical practitioners.




