7 Real-Life Medical Scribe Note Examples for Effortless Documentation
Back-to-back appointments and a looming mountain of documentation.
That's no one's favorite feeling.
What if you could manage your documentation so efficiently that you can relax, pursue your hobbies, or simply enjoy dinner with your family without the shadow of pending paperwork?
Learning from real-life medical scribe note examples can make this your reality. The more examples you study, the more you can fast-track medical documentation.
The result? Clear and accurate notes in minutes.
That’s why we’ve curated seven examples of medical scribe notes with tips to use each type of documentation for the right use case. You'll find real-life examples and a list of elements to structure each note.
The 7 most common types of medical scribe notes
Healthcare providers already have enough on their plates without the added pressure of inefficient documentation.
With burnout rates climbing — research indicates that 49% of providers face burnout — it's time to investigate the documentation process.
We’ll help you steer away from this stress with seven examples of medical scribe notes, each one with hands-on guidelines.
1. History and physical (H&P) examination
When it’s used
- New patient consultations or hospital admissions
- Preoperative assessments and evaluations
- Complex or chronic cases requiring follow-up visits
An H&P is comprehensive documentation on a patient’s health issues when they visit a physician for the first time. Medical scribes also create these notes during follow-up medical checks.
Here’s a quick snapshot of what these notes typically look like:
When creating H&P notes, it's crucial that you:
- Prioritize clarity in the HPI details: Chronologically document a patient's symptoms, including onset, intensity, duration, and potential triggers. Highlight any factors that alleviate their symptoms.
- Contextualize the information: Provide more insights about the recorded data based on the patient’s stated issue. For example, “Patient is a 33-year-old male with a history of chronic GERD, manifesting as severe epigastric pain after meals.”
- Tie assessments to the CC: All clinical findings, including results from the PE and ROS, should be evaluated based on the primary complaint. That said, don’t skip additional observations that may seem unrelated to the condition.
- Document specific treatment timeframes: Note the exact dosage, frequency, and follow-up routines for prescribed medication. For example, "Prescribed 10 mg omeprazole daily for 3 weeks. Follow up in 1 week."
Additionally, you want to include the treatment or management steps for confirmed diagnoses. This simplifies your communication with patients and informs them of therapeutic or preventive lifestyle changes as soon as possible.
Key sections typically recorded in H&P notes
2. Consultation notes
When it’s used
- To further evaluate a patient’s condition or confirm a diagnosis
- For seeking specialist expertise or guidance on complex medical cases
Consultation notes are typically created when the primary physician wants to seek the clinical opinion of a specialist in assessing or treating a patient’s condition.
These clinical notes must be concise while presenting all the relevant details to the specialist.
A perfect example would look something like this:

Here are some points to remember when creating consultation notes:
- Start with the exact reason: Specify the question or issue the referring physician wants the specialist to address. This gives the specialist a clear direction to assess the patient's condition.
- Provide a detailed but concise patient history: Include only the most relevant clinical information from the patient's medical history. Comorbid conditions or past surgeries related to the illness all fall in this category.
- Inform the consultant about previously administered PEs: Include data from already administered tests to make the referral more effective. You can also present any findings from your ROS report related to the referral question.
It's best to update the information based on the physician's recommended timelines for complex cases. If the patient's condition is critical, mention it on the note.
Key sections typically recorded in consultation notes
3. Diagnostic test or lab result documentation
When it’s used
- While ordering diagnostic assessments
- During routine patient visits
- For monitoring ongoing treatment plans or reviewing disease progression
One of the core responsibilities of a medical scribe is documenting the findings from diagnostic or lab tests. This also includes noting and interpreting results from such clinical examinations.
Here's what diagnostic or lab results look like in most cases:

When recording the results from a diagnostic or imaging report, ensure that you:
- Organize test information: Structure the data on the administered test for maximum clarity. Consider organizing/presenting the information based on test types or using concise headings (Radiology Report/CBC/etc).
- Contextualize the results: While noting the test results, always contextualize the findings based on clinical significance. For example, "Elevated ALT and AST indicate liver injury. Viral hepatitis suspected."
You also need to record follow-up instructions. For example, if the lab results suggest a need for further testing, you must note specific actions to be taken next. Here’s an example: "Repeat CBC in 2 weeks to assess for any improvements in hemoglobin level."
Key sections typically recorded in diagnostic tests
4. Progress notes
When it’s used
- In follow-up consultations for chronic conditions (diabetes/epilepsy/etc.)
- During routine clinic rounds
- For systematically monitoring treatment efficacy or progression of the condition
Progress notes record a patient's current clinical status, response to ongoing medical care, or changes in their existing conditions/symptoms.
Here are three main types of progress notes:
- SOAP note: Subjective, Objective, Assessment, and Plan notes document a patient’s progress over time in a structured format.
- DAP note: Data, Assessment, and Plan format combines the patient’s subjective information and the physician’s objective assessment into one section (Data).
- DART note: Data, Action, Response, and Treatment notes are usually applied in a psychiatric setting.
Progress notes include extensive details about a patient’s current mental and physical health.
Here are a few tips to create such notes:
- Be consistent: Typically, progress notes are created daily. You should make sure that the data is updated consistently and reflects the patient’s present clinical status. This prevents errors in treatment administration and prolonged recovery periods.
- Track all changes: Record any new developments in the patient's condition since the last progress note. This can be as simple as "Patient reports less pain after today's physical therapy session."
- Add actionable updates for each subsequent note: Each progress note you create should also clearly define follow-up actions. For instance, “Patient’s culture report confirms amoxicillin sensitivity. Discontinue IV antibiotics from hereon.”
To get a better understanding here, take a look at this progress note (in SOAP format):
Key sections typically recorded in progress notes
5. Preoperative and postoperative evaluation notes
When it’s used
- Before undergoing surgery to review the patient’s overall health
- To determine the patient’s readiness for the procedure
Before surgical procedures, medical scribes create a comprehensive health record for a patient. This includes their medical history, test results from physical examinations or diagnostic tests, and the proposed operative method.
These notes are updated post-surgery to include the patient’s immediate health/clinical status and an assessment of the recovery period.
While preoperative and postoperative evaluation notes are created asynchronously, you can consolidate these documents to provide a comprehensive overview of the patient's condition.
Here’s a part of a preoperative evaluation note:
Here are three of the most important points to remember when creating preoperative/postoperative evaluation notes:
- Detail all risk factors: Document all elements that can pose a risk to the patient during the procedure. This includes comorbidities (diabetes/hypertension), medications (anticoagulants, etc), and the patient's functional state.
- Record instructions for specific operative difficulties: If there are patient-specific challenges (history of difficult intubation, etc), clearly record them in your notes. Also, detail the physician’s recommendation for managing such concerns.
- Elaborate on postoperative complications: It's crucial to record, contextualize, and detail the next steps for post-surgery concerns. For example, "Patient's postoperative fever is likely due to atelectasis. Start low-dose heparin for DVT prophylaxis."
It also helps to document expected recovery milestones and the patient's current progress. A straightforward example would be: "Patient can move with minimal assistance. Follow up in 1 week for suture removal."
Key sections typically recorded in preoperative and postoperative notes
6. Procedure notes
When it’s used
- After any surgical (invasive and non-invasive) operation
- Post non-surgical interventions (biopsies/endoscopies/etc.)
During surgical operations, scribes have to note down details of the procedure, like its exact steps, potential complications, and any relevant medical findings.
Procedure notes are often the most challenging to create. This is primarily due to the extensive technical knowledge they require.
Here are three tips to make things easier on yourself:
- Be specific about operative steps: Accurately note every critical surgery step. This includes the surgical approach, specific incisions made, and technique variations.
- Document any intraoperative findings: Record any surgical complications and corrective actions in detail in your notes. For instance, "Adhesions were found in the lower left quadrant during the laparotomy. Additional dissection was required".
- Use clear and concise language: While operative notes are significantly technical, avoid any unnecessary jargon and be precise about what was performed. Here's an example: "Performed a right nephrectomy due to suspected renal malignancy."
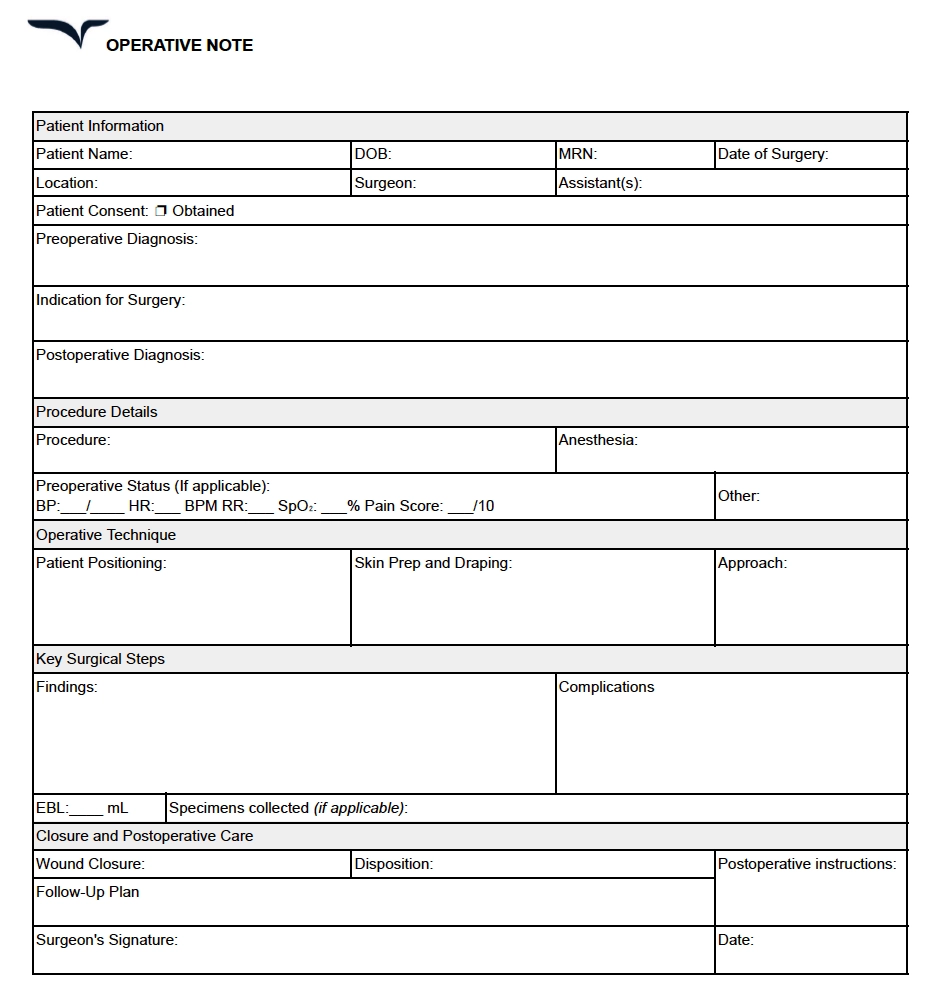
For a better reference, here’s a basic sample of a procedure note:
Key sections typically recorded in operative or procedure notes
7. Discharge summaries
When it’s used
- Upon discharge from a hospital or an in-patient facility
Before a patient is discharged, you have to document the treatment course administered, including a final diagnosis. These notes also mention follow-up care instructions for managing chronic conditions.
Here’s a sample of what these discharge summaries typically look like:
Consider these tips when creating discharge summaries:
- Record and summarize the entire course: Detail all interventions during the hospitalization period. Additionally, maintain an accurate record of the patient's progress and condition upon discharge.
- List all prescribed medications: Comprehensively list the administered and ongoing medication. Also, elaborate on any instructions. For example, "Prescribed 500 mg amoxicillin once a day for 1 week. Take with food to reduce GI issues.”
- Clarify post-discharge plans and follow-up actions: Note any referrals for physical therapy, community resources, or post-discharge recommendations. For instance, "Consultation with cardiology in 2 weeks to assess postoperative recovery".
Another tip would be to document patient communication in your notes.
Confirm that the patient understands the discharge/follow-up plan in its entirety. This can be reflected in your records as a simple "verbalized understanding with patient."
Key sections typically recorded in discharge summaries
Make your life (and documentation) easier with an AI scribe
Imagine the relief of ending a packed day at the clinic and realizing you don’t have to spend hours charting every visit.
That’s life with Freed.
The AI medical scribe exists to win back time and make life easier for clinicians like you.

Record patient conversations with the click of a button and Freed will prepare detailed and clinically accurate notes based on your preferences and specialty.
Simplify medical documentation for yourself
Creating accurate clinical notes has always been a tedious task.
But not anymore.
This article gives you a handy list of medical scribe note examples with actionable tips to create these documents effortlessly.
AI scribes like Freed take away the stress of manually documenting every patient visit. Simply record all interactions and leave it on Freed to create notes instantly, accurately.
Sign up for a free trial to see it yourself.
Table of Contents
Back-to-back appointments and a looming mountain of documentation.
That's no one's favorite feeling.
What if you could manage your documentation so efficiently that you can relax, pursue your hobbies, or simply enjoy dinner with your family without the shadow of pending paperwork?
Learning from real-life medical scribe note examples can make this your reality. The more examples you study, the more you can fast-track medical documentation.
The result? Clear and accurate notes in minutes.
That’s why we’ve curated seven examples of medical scribe notes with tips to use each type of documentation for the right use case. You'll find real-life examples and a list of elements to structure each note.
The 7 most common types of medical scribe notes
Healthcare providers already have enough on their plates without the added pressure of inefficient documentation.
With burnout rates climbing — research indicates that 49% of providers face burnout — it's time to investigate the documentation process.
We’ll help you steer away from this stress with seven examples of medical scribe notes, each one with hands-on guidelines.
1. History and physical (H&P) examination
When it’s used
- New patient consultations or hospital admissions
- Preoperative assessments and evaluations
- Complex or chronic cases requiring follow-up visits
An H&P is comprehensive documentation on a patient’s health issues when they visit a physician for the first time. Medical scribes also create these notes during follow-up medical checks.
Here’s a quick snapshot of what these notes typically look like:
When creating H&P notes, it's crucial that you:
- Prioritize clarity in the HPI details: Chronologically document a patient's symptoms, including onset, intensity, duration, and potential triggers. Highlight any factors that alleviate their symptoms.
- Contextualize the information: Provide more insights about the recorded data based on the patient’s stated issue. For example, “Patient is a 33-year-old male with a history of chronic GERD, manifesting as severe epigastric pain after meals.”
- Tie assessments to the CC: All clinical findings, including results from the PE and ROS, should be evaluated based on the primary complaint. That said, don’t skip additional observations that may seem unrelated to the condition.
- Document specific treatment timeframes: Note the exact dosage, frequency, and follow-up routines for prescribed medication. For example, "Prescribed 10 mg omeprazole daily for 3 weeks. Follow up in 1 week."
Additionally, you want to include the treatment or management steps for confirmed diagnoses. This simplifies your communication with patients and informs them of therapeutic or preventive lifestyle changes as soon as possible.
Key sections typically recorded in H&P notes
2. Consultation notes
When it’s used
- To further evaluate a patient’s condition or confirm a diagnosis
- For seeking specialist expertise or guidance on complex medical cases
Consultation notes are typically created when the primary physician wants to seek the clinical opinion of a specialist in assessing or treating a patient’s condition.
These clinical notes must be concise while presenting all the relevant details to the specialist.
A perfect example would look something like this:

Here are some points to remember when creating consultation notes:
- Start with the exact reason: Specify the question or issue the referring physician wants the specialist to address. This gives the specialist a clear direction to assess the patient's condition.
- Provide a detailed but concise patient history: Include only the most relevant clinical information from the patient's medical history. Comorbid conditions or past surgeries related to the illness all fall in this category.
- Inform the consultant about previously administered PEs: Include data from already administered tests to make the referral more effective. You can also present any findings from your ROS report related to the referral question.
It's best to update the information based on the physician's recommended timelines for complex cases. If the patient's condition is critical, mention it on the note.
Key sections typically recorded in consultation notes
3. Diagnostic test or lab result documentation
When it’s used
- While ordering diagnostic assessments
- During routine patient visits
- For monitoring ongoing treatment plans or reviewing disease progression
One of the core responsibilities of a medical scribe is documenting the findings from diagnostic or lab tests. This also includes noting and interpreting results from such clinical examinations.
Here's what diagnostic or lab results look like in most cases:

When recording the results from a diagnostic or imaging report, ensure that you:
- Organize test information: Structure the data on the administered test for maximum clarity. Consider organizing/presenting the information based on test types or using concise headings (Radiology Report/CBC/etc).
- Contextualize the results: While noting the test results, always contextualize the findings based on clinical significance. For example, "Elevated ALT and AST indicate liver injury. Viral hepatitis suspected."
You also need to record follow-up instructions. For example, if the lab results suggest a need for further testing, you must note specific actions to be taken next. Here’s an example: "Repeat CBC in 2 weeks to assess for any improvements in hemoglobin level."
Key sections typically recorded in diagnostic tests
4. Progress notes
When it’s used
- In follow-up consultations for chronic conditions (diabetes/epilepsy/etc.)
- During routine clinic rounds
- For systematically monitoring treatment efficacy or progression of the condition
Progress notes record a patient's current clinical status, response to ongoing medical care, or changes in their existing conditions/symptoms.
Here are three main types of progress notes:
- SOAP note: Subjective, Objective, Assessment, and Plan notes document a patient’s progress over time in a structured format.
- DAP note: Data, Assessment, and Plan format combines the patient’s subjective information and the physician’s objective assessment into one section (Data).
- DART note: Data, Action, Response, and Treatment notes are usually applied in a psychiatric setting.
Progress notes include extensive details about a patient’s current mental and physical health.
Here are a few tips to create such notes:
- Be consistent: Typically, progress notes are created daily. You should make sure that the data is updated consistently and reflects the patient’s present clinical status. This prevents errors in treatment administration and prolonged recovery periods.
- Track all changes: Record any new developments in the patient's condition since the last progress note. This can be as simple as "Patient reports less pain after today's physical therapy session."
- Add actionable updates for each subsequent note: Each progress note you create should also clearly define follow-up actions. For instance, “Patient’s culture report confirms amoxicillin sensitivity. Discontinue IV antibiotics from hereon.”
To get a better understanding here, take a look at this progress note (in SOAP format):
Key sections typically recorded in progress notes
5. Preoperative and postoperative evaluation notes
When it’s used
- Before undergoing surgery to review the patient’s overall health
- To determine the patient’s readiness for the procedure
Before surgical procedures, medical scribes create a comprehensive health record for a patient. This includes their medical history, test results from physical examinations or diagnostic tests, and the proposed operative method.
These notes are updated post-surgery to include the patient’s immediate health/clinical status and an assessment of the recovery period.
While preoperative and postoperative evaluation notes are created asynchronously, you can consolidate these documents to provide a comprehensive overview of the patient's condition.
Here’s a part of a preoperative evaluation note:
Here are three of the most important points to remember when creating preoperative/postoperative evaluation notes:
- Detail all risk factors: Document all elements that can pose a risk to the patient during the procedure. This includes comorbidities (diabetes/hypertension), medications (anticoagulants, etc), and the patient's functional state.
- Record instructions for specific operative difficulties: If there are patient-specific challenges (history of difficult intubation, etc), clearly record them in your notes. Also, detail the physician’s recommendation for managing such concerns.
- Elaborate on postoperative complications: It's crucial to record, contextualize, and detail the next steps for post-surgery concerns. For example, "Patient's postoperative fever is likely due to atelectasis. Start low-dose heparin for DVT prophylaxis."
It also helps to document expected recovery milestones and the patient's current progress. A straightforward example would be: "Patient can move with minimal assistance. Follow up in 1 week for suture removal."
Key sections typically recorded in preoperative and postoperative notes
6. Procedure notes
When it’s used
- After any surgical (invasive and non-invasive) operation
- Post non-surgical interventions (biopsies/endoscopies/etc.)
During surgical operations, scribes have to note down details of the procedure, like its exact steps, potential complications, and any relevant medical findings.
Procedure notes are often the most challenging to create. This is primarily due to the extensive technical knowledge they require.
Here are three tips to make things easier on yourself:
- Be specific about operative steps: Accurately note every critical surgery step. This includes the surgical approach, specific incisions made, and technique variations.
- Document any intraoperative findings: Record any surgical complications and corrective actions in detail in your notes. For instance, "Adhesions were found in the lower left quadrant during the laparotomy. Additional dissection was required".
- Use clear and concise language: While operative notes are significantly technical, avoid any unnecessary jargon and be precise about what was performed. Here's an example: "Performed a right nephrectomy due to suspected renal malignancy."
For a better reference, here’s a basic sample of a procedure note:
Key sections typically recorded in operative or procedure notes
7. Discharge summaries
When it’s used
- Upon discharge from a hospital or an in-patient facility
Before a patient is discharged, you have to document the treatment course administered, including a final diagnosis. These notes also mention follow-up care instructions for managing chronic conditions.
Here’s a sample of what these discharge summaries typically look like:
Consider these tips when creating discharge summaries:
- Record and summarize the entire course: Detail all interventions during the hospitalization period. Additionally, maintain an accurate record of the patient's progress and condition upon discharge.
- List all prescribed medications: Comprehensively list the administered and ongoing medication. Also, elaborate on any instructions. For example, "Prescribed 500 mg amoxicillin once a day for 1 week. Take with food to reduce GI issues.”
- Clarify post-discharge plans and follow-up actions: Note any referrals for physical therapy, community resources, or post-discharge recommendations. For instance, "Consultation with cardiology in 2 weeks to assess postoperative recovery".
Another tip would be to document patient communication in your notes.
Confirm that the patient understands the discharge/follow-up plan in its entirety. This can be reflected in your records as a simple "verbalized understanding with patient."
Key sections typically recorded in discharge summaries
Make your life (and documentation) easier with an AI scribe
Imagine the relief of ending a packed day at the clinic and realizing you don’t have to spend hours charting every visit.
That’s life with Freed.
The AI medical scribe exists to win back time and make life easier for clinicians like you.

Record patient conversations with the click of a button and Freed will prepare detailed and clinically accurate notes based on your preferences and specialty.
Simplify medical documentation for yourself
Creating accurate clinical notes has always been a tedious task.
But not anymore.
This article gives you a handy list of medical scribe note examples with actionable tips to create these documents effortlessly.
AI scribes like Freed take away the stress of manually documenting every patient visit. Simply record all interactions and leave it on Freed to create notes instantly, accurately.
Sign up for a free trial to see it yourself.
FAQs
Frequently asked questions from clinicians and medical practitioners.
What to put in medical notes?
How do you write a medical note?
How accurate is an AI SOAP note generator with medical terminology?
Can a clinical documentation platform actually adapt to my specialty?
Related content






.avif)



